A Holistic Approach to Clinical Revenue Cycle
In my experience, the clinical revenue cycle (CRC) is seldom mentioned and under-reported. The more universally recognized concept, of course, is revenue cycle management (RCM). It is the umbrella of which CRC is an integral part and a crucial revenue driver, accounting for a large portion of the direct and indirect cost of providing care. CRC needs to be recognized for this importance, and also requires improvement from its present status with a more holistic approach.
What is Revenue Cycle Management?
As is well-known in its simplest definition, RCM is the financial process that includes administrative and clinical functions that contribute to the identification, capture, management, and collection of patient service revenue – essentially, the entire life cycle of the patient account, from creation to payment.

Although RCM is said to include clinical functions, the financial nuances of the CRC seem to be rarely included in detail.
What is Clinical Revenue Cycle?
CRC is the summation of the clinical side of an organization, including the direct cost of patient care and the indirect cost of the overhead to deliver that care. The business side of healthcare is essential to ensure facility survival, especially in today’s world of decreasing profit margins. Yet how the crucial functions of the clinical side influence the overall revenue cycle is so poorly understood, even though they must operate in tandem. Clinical departments and physicians have a responsibility for assessing and documenting the complexity of care rendered to reflect and justify their services and provide proper navigation of the care, in order to preserve and protect sustainable revenue.
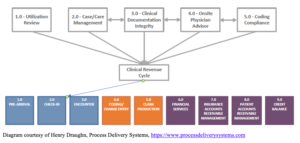
There are various models out there, but none that support a holistic approach to help lead a facility to realize unrecorded but rightfully earned revenue. Keep in mind that with holism, none of the five components listed below are more important than any other component – or more important than the whole. They are asymmetrical, as far as function and process, but must be balanced across the continuum of clinical revenue cycle to yield the best results, with knowledge sharing and collaboration.
Why is it Important?
As noted, the components of clinical revenue cycle are not symmetrical. CRC will function best when these asymmetries are balanced during function, because if our systems become overused and dominated by one pattern, unintended consequences can occur, and one can see that in team workarounds, where bottlenecks and constraints arise in the processes. If not addressed, it will build over time, with potentially cumulative problems, until collaboration is instituted. There are five asymmetrical teams – silos, if you will – and each is part of a system with unique demands and distinctive functions, in differing situations. With a holistic approach, it is essential to realize that no one component is more important than any other or the whole. There is a common element to all components, a connecting factor of documentation, that holds it all together. Documentation provides a consistent, centralized platform to be utilized for multiple purposes by each component.
Even with the few models of CRC that exist, none cite the components that must work together and have the most effect on potential revenue.

Diagram courtesy of Henry Draughn, Process Delivery Systems, https://www.processdeliverysystems.com
The five component definitions of CRC are the following:
- Utilization Review – This is the process of reviewing an episode of care, and confirming that the payor will provide appropriate financial coverage for the items and medical services In reality, the care provided has nothing to do with the level-of-care determination, but the payment is influenced by acuity, the medical necessity, as judged by the documentation of same.
- Care/Case Management – According to the Case Management Society of America (CMSA), this is a collaborative process of assessment, planning, facilitation, carecoordination, evaluation, and advocacy for options and services to meet individual and family comprehensive health This is sometimes summarized as the progression of care.
- Clinical Documentation Integrity (CDI) – This is the process of improving healthcarerecords to ensure improved patient outcomes, data quality, and documentation to support accurate reimbursement. It can involve physician conversations and education for accuracy and specificity.
- Physician Advisor – This role supports utilization review in recommending appropriate level of care, collaborating with case management and CDI, and performing other various duties.
- Coding – This is the process by which medicalprocedures and diagnoses are represented and displayed by universal code numbers for the purposes of appropriate reimbursement.
The Importance and Relevance of CRC in RCM
There are many important and relevant reasons for these clinical factors playing a crucial role in overall revenue cycle management, and in dealing with the direct cost of care provision and indirect cost of overhead. As an example, with utilization review, getting the patient into the correct level of care with the proper documentation of acuity can have significant financial consequences. Depending on the considerable difference in payment between inpatient and observation status, placing a patient in observation who would have qualified as an inpatient would be a loss of that additional payment to the facility, depending on the payer. Collateral effects include the increased financial burden to a Medicare beneficiary, artificial increase in length of stay (LOS) and mortality rates, and lack of eligibility for skilled nursing placement. This is just one example, and the list goes on with the role of each of the components.
Since CRC is so critical and variable to overall RCM, where does it fit into the grand scheme? It is actually the episode of care itself.
What is the Role of CRC?
The overall goal of RCM is to develop processes for accuracy of information, specificity of detail, and protection of earned revenue. There are two parts to this, and these include the following:
- Information-gathering that can be automated, such as registration, charge entry, claim production, etc. This is fairly constant.
- Clinical variations that affect and determine those end results, the charges that are billed, aiding in accurate coding, as well as reduction in denials and clawbacks of deserved revenue.
Once a goal – the outcome – is established, it then becomes important to determine the outputs needed to get there. Let’s help with these basic definitions:
- The outcomesare what the business wants or needs to achieve, or more simply, the results.
- The outputsare the actions or items that contribute to achieving an outcome. Remember:
- Monitor the process, not the tasks.
It has been mentioned that CRC is composed of asymmetrical units that may tend to operate in silos, making a holistic approach and cross-functionality somewhat challenging. On the other hand, there is a connecting factor for all of the elements of CRC, and that is the documentation that exists in the medical record. In real estate, the three key words are location, location, location. In healthcare it is documentation, documentation, documentation. Every single element of CRC depends on documentation. Documentation provides a consistent, centralized platform to be utilized for multiple purposes. Physician documentation is paramount, and many times it presents the biggest challenge in the process that CRC needs to address.
Proper documentation must:
- Accurately tell the patient story;
- Define the acuity – the who, what, when, why, and how – for each episode of care;
- Support favorable medical review decisions;
- Ensure that the items and services were medically necessary and were actually provided and performed;
- Provide support for accurate coding on claims submitted; and
- Become the key factor to reduce and overturn denials.
Indicators of Success
Clinical revenue cycle has the greatest chance of success when it is successfully integrated into the revenue cycle umbrella and fully supported by leadership and management. The business of healthcare cannot be left up to only financially oriented individuals, as the main business of healthcare is to provide appropriate care to patients, and it must be documented. That is the essential requirement of the clinical side.
RCM appropriately starts with the components that begin prior to the actual day of admission and can continue after discharge. CRC begins at the time of admission and ends with the day of discharge. That interim period of time and activity can and does have a huge impact on revenue.
A process improvement specialist, whether internal or external, is needed to diagnose and recommend an integrative holistic approach of the various components of CRC, balancing the asymmetries to allow for successful movement and function. But, again, recognition, not denial, must occur before the correct process can be instituted.

